
Monkeypox
Monkeypox is a member of the same family of viruses (variola virus) that causes smallpox. Because of this close relationship, all the current therapies and vaccines for monkeypox were actually developed and authorized for smallpox. Monkeypox is not related to chickenpox. Monkeypox was discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of research monkeys. The first human case of monkeypox was recorded in 1970. This virus is usually found in Africa, though there has been a fast-growing outbreak in the United States since May 2022.
Transmission: Monkeypox is spread in humans primarily from direct contact with the virus from an infected person’s skin sores, scabs, or body fluids. It can be spread indirectly, to a lesser degree through materials contaminated with the virus. Transmission from respiratory secretions likely requires oral lesions and prolonged close contact. Animal to human spread can occur from an infected animal’s body fluids or bite.
Most reported cases have occurred in persons who have had close, sustained, intimate skin-to-skin contact with the lesions (or fluid from lesions) from an infected person.
The CDC reports that most cases of monkeypox in the U.S. have occurred among gay, bisexual, trans, and other men who have sex with men (MSM). At the time of this post, the number of monkeypox cases are doubling on a weekly basis. At the current rate, it is more than likely the condition will extend to the general public. The take home message, regardless of one’s sexual orientation, is to avoid social settings that bring people in close skin-to-skin contact (crowded dance floors, music festivals, etc.) or intimacy with a person who has an unexplained rash.
Monkeypox is not spread easily from person to person through casual contact. The overall risk to the public is low and will remain so as long as they are mindful of the conditions that spread the virus.
It is currently not known:
- If the virus can be spread when someone has no symptoms.
- Whether monkeypox can be spread through semen, vaginal fluids, urine, or feces.
- What degree can monkeypox can be spread through respiratory secretions.
Clinical Illness: The incubation period (time from exposure to the virus to the time first symptoms appear) varies from 5 days to as long as 21 days. For the current outbreak, the mean incubation period is 8.5 days, during which time the person feels fine and does not have symptoms.
Symptoms: The initial set of symptoms (prodrome) are the development of flu-like symptoms (fever, chills, headache, swollen lymph nodes, severe fatigue) with the characteristic rash appearing 1-4 days later. Some persons can develop the rash prior to the flu-like symptoms, while others just develop a rash as the only manifestation of the infection.
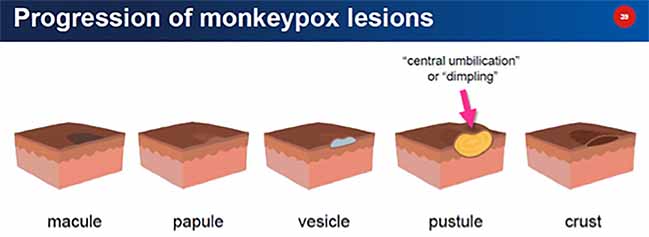
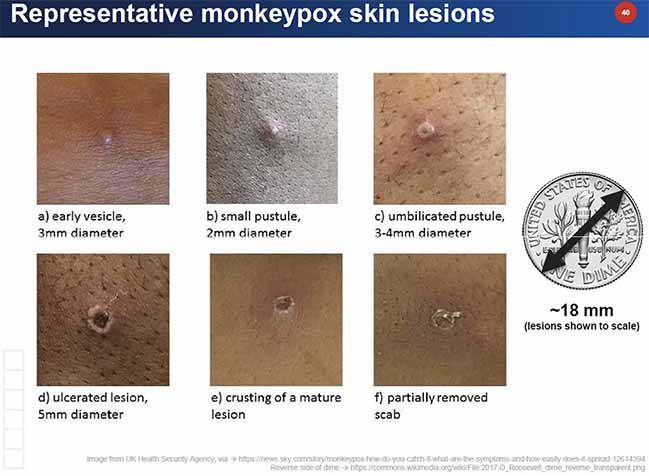
The typical rash progresses through several stages over 1-2 weeks: the rash begins with pink macules (round, flat lesions, 2-5 mm diameter), which progress to raised, round fleshy bumps (papules), to fluid-filled lesions (vesicles), to cloudy-fluid filled raised lesions (pustules), often with a central dimple “umbilication”, followed by the lesion drying up and scabbing.
Persons with flu-like symptoms who do not develop a rash by day 5 are unlikely to have monkeypox.
Monkeypox may be spread during the prodromal stage (fever, lymphadenopathy, etc.), but is most contagious with the appearance of the rash, where one can spread the virus until the rash has healed, all scabs have fallen off, and a fresh layer of skin has formed. The illness typically lasts 2-4 weeks.

Prevention:
1. Vaccination: Two smallpox vaccines, modified vaccinia Ankara/MVA (JYNNEOS) and ACAM2000 have shown efficacy at preventing monkeypox. MVA (JYNNEOS) is a highly attenuated, nonreplicating vaccinia virus that is at least 85 % effective. This vaccine is available in limited supply through SC DHEC for high risk individuals who meet the following criteria:
- Are age 18 or older.
- Identify as a gay or bisexual man, trans man, transgender, gender-fluid or gender nonconforming individual who has sex with men.
- Have had multiple male sexual contacts within the last two weeks.
- To make an appointment, call DHEC’s CareLine at 1-855-472-3432.
2. Behavioral Measures include the following: See CDC for more information on preventive measures:
- Avoid close, skin-to-skin contact with anyone has a rash that looks like monkeypox.
- Don’t touch the rash or scabs of a person with monkeypox.
- Don’t kiss, hug, cuddle or have sex with someone with monkeypox.
- Don’t share eating utensils or cups with a person with monkeypox.
- Avoid handling or touching the bedding, towels or clothing of a person with monkeypox.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer.
What should I do if I think I may have been exposed to monkeypox? Most persons can safely continue their day-to-day activities over the following 21 days and self-monitor for flu-like symptoms (including twice daily temperature checks) and the appearance of a rash. They should self-isolate with the appearance of any symptoms and report their condition to their healthcare provider for guidance. Currently there are no commercial tests that can detect monkeypox during the incubation period. Certain prophylactic measures may be appropriate for high-risk exposures.
What should I do if I have had intimate exposure to a person with diagnosed monkeypox infection? Persons with significant high-risk exposure to persons with active monkeypox infection may be eligible to receive a smallpox vaccine which can lessen the severity of the illness. Experts believe that the smallpox vaccine (JYNNEOS), when given within 4 days of exposure, may prevent the disease. When given 4-14 days after exposure may lessen the severity of the illness. The vaccine is most effective when given at the earliest time after an exposure (< 4 days), with diminishing benefits thereafter. Contact SC DHEC @ 1-855-472-3432 if interested in learning more about this option.
What should I do if I have an unexplained rash that I am worried might be monkeypox? Until the rash can be evaluated, avoid touching the rash, and keep the rash covered with gauze if it is located at an exposed area of skin and/or is draining fluid. Wash your hands thoroughly with soap and water if you have touched the rash. Call ahead to the clinic you wish to be evaluated and let them know your concern, to make sure they have the laboratory sampling material necessary to make a diagnosis, as well the personal protective equipment for their clinical staff. MUSC Student Health is available by appointment for consultation and/or in-person evaluation (843) 792-3664.
What treatments are available for monkeypox?
Most healthy individuals will have an uneventful clinical course that will resolve over 2-4 weeks with only symptomatic treatment.
Treatment can be considered in persons with severe illness or who are and at risk for severe illness. Those include children less than 8 years old, pregnant women, people with skin conditions like eczema and immunocompromised individuals. All current treatments were developed and approved for treatment of smallpox and no large- scale human studies for treatment of monkeypox have been conducted.
- Tecovirimat is an antiviral agent that inhibits the activity of proteins necessary for formation of the viral envelope and propagation of this virus. When given early in the infection, animal studies have shown to have decreased the risk of dying.
- Vaccinia Immune Globulin Intravenous (VIGIV) - Can be considered for prophylactic use in an exposed person with severe immunodeficiency in T-cell function for which smallpox vaccination following exposure to monkeypox virus is contraindicated.
- Cidofovir/Brincidofovir - antiviral agents that blocks the enzyme DNA polymerase which is necessary for DNA synthesis and viral replication. Similar agents are currently used to treat herpes and CMV in humans (acyclovir, valacyclovir). In vitro and animal studies show efficacy, though it is unknown if they are beneficial for monkeypox in humans.
Resources:
MUSC Catalyst article 7/18/2022 “As number of monkeypox cases rises, infectious diseases expert predicts more to come”
MUSC Catalyst article 7/29/2022 “MUSC works with DHEC to get the word out on monkeypox”
CDC: Monkeypox
SC DHEC: Main Website: Monkeypox
